



Peripheral Artery Disease (PAD) is a common but serious condition affecting millions of people in India. The prevalence of PAD is notably high, with studies revealing that it affects around 10-20% of adults aged 40 years and above. This rate increases significantly with age, particularly among those over 70 years old, as well as individuals with a history of diabetes or smoking.
PAD can cause significant discomfort and increase the risk of severe complications such as foot gangrene and diabetic foot ulcers. Timely intervention is crucial to prevent these outcomes, and one of the most effective treatments for PAD is the combination of angioplasty and stenting. Read on to learn how these procedures work and the benefits they offer to patients with PAD.

PAD is a disease characterised by the narrowing or blockage of the arteries, particularly in the legs. This narrowing is typically caused by atherosclerosis, a process in which fatty deposits, or plaques, build up on the walls of the arteries. As these plaques grow, they reduce the space available for blood to flow, leading to lower oxygen and nutrients being supplied to the tissues in the legs. PAD can cause significant discomfort and increase the risk of severe complications such as foot gangrene and diabetic foot ulcers. If left untreated, it can cause tissue death and the need for amputation.
Several factors can increase the risk of developing PAD. Atherosclerosis is the primary cause, but other risk factors include:
The symptoms of PAD can differ depending on the severity of the condition. In the early stages, many people may not experience any symptoms, but as the disease progresses, the following signs may become apparent:
Diagnosis of PAD generally involves a combination of medical history, physical examination, and diagnostic tests. Common tests used to diagnose PAD include:
Once PAD is diagnosed, treatment focuses on managing symptoms, increasing quality of life, and preventing complications. Treatment options include:
Angioplasty and stenting are minimally invasive methods used to treat PAD.
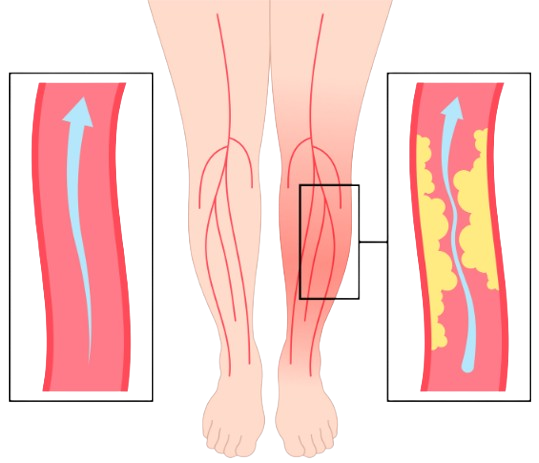
Angioplasty is a minimally invasive method used to widen narrowed or blocked arteries. A narrow catheter tube is inserted into the affected artery during this procedure. The catheter has a small balloon on its tip, which is inflated to push the plaque against the artery walls, widening the artery and restoring blood flow. The balloon is then deflated and taken out, leaving the artery open.
Angioplasty is often recommended for patients with PAD who have not responded to lifestyle changes and medications or those at risk of developing complications such as foot gangrene or diabetic foot ulcers.
Stenting involves placing a small mesh tube, known as a stent, in the artery to keep it open after angioplasty. The stent acts as a scaffold, stopping the artery from narrowing again. There are two main types of stents:
Stents are usually placed during or after angioplasty to maintain blood flow and reduce the risk of artery narrowing again.
Angioplasty and stenting are often performed together as part of a comprehensive treatment plan for PAD. The combination of these procedures enhances treatment efficacy and patient outcomes. The process typically involves:
This combination improves circulation, reduces symptoms, and prevents serious complications like foot gangrene and diabetic foot ulcers.
Angioplasty and stenting offer several benefits for Patients with PAD, including:
Following angioplasty and stenting, proper post-procedure care is essential for a successful recovery. This includes:
Peripheral Artery Disease is a serious ailment that requires timely intervention to prevent severe complications such as foot gangrene and diabetic foot ulcers. Angioplasty and stenting are effective, minimally invasive treatments that can significantly improve circulation and reduce the risk of complications. Early diagnosis and treatment are necessary for managing PAD effectively.
If you're experiencing symptoms of PAD or are at risk of the condition, don't let it control your life. Dr Akhil Monga provides expert treatment for such conditions. Book an appointment with him today for a comprehensive evaluation and personalised treatment plan. He will help you regain mobility, reduce pain, and improve your life.